Rachel had an MRI scan on Wednesday night. The techs had a lot of difficulty finding her veins to inject the contrast. 7 needle sticks later, they were finally able to get it in and finish the MRI. We got home around 11pm (after an 8:30pm start to the MRI) and Rachel’s poor hand was really hurting after all the needle sticks (3 in one arm, 3 in one hand, and the final successful one in the other arm.) The frustrating thing is that she has a port that could be used for this, but radiology isn’t allowed to access ports. I asked if one of the nurses from pediatrics could come downstairs to do it, but they’re not allowed to have anyone else do any procedures on the radiology patients “for charting purposes.” So frustrating! She was accessed that morning by her home nurse too, to do her blood test, but she de-accessed her right after. It would have probably made the EKG and echocardiogram a bit difficult to do if she was accessed anyway. They used the veins in her arms on Monday for the bone scan contrast and blood test with no problems at all, too.
On Thursday, Rachel had her pre-op appointment with the main doctors on her surgical team, which includes Dr. Joseph Schwab, an orthopedic oncologist specializing in spinal tumors, Dr. Thomas Delaney, a radiation oncologist, and Branko Bojovic, a plastic surgeon. Not wanting to leave them out, Rachel’s primary pediatric oncologist here in Maine is Dr. Aaron Weiss, and her pediatric oncologist in Boston is Dr. David Ebb. Her neurosurgeon back in November was Dr. Joseph Alexander.
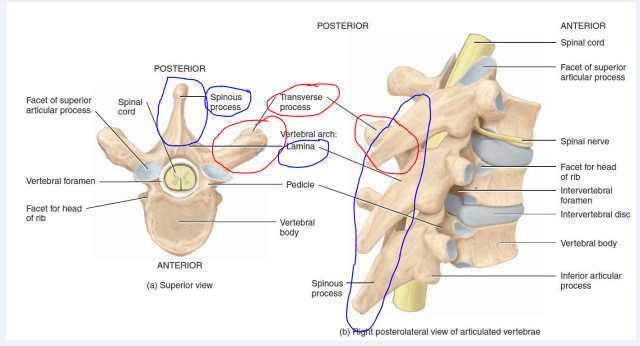
For those of you interested in the technical medical details, Rachel’s first surgery back in November was a laminectomy of the thoracic vertebrae T3 through T5, which means they removed the lamina and spinous process (the bumpy part of your spine that you can feel under your skin) of those 3 vertebrae in addition to the tumor. The remaining cancer cells are on the transverse process of the T4 vertebra, so next month’s surgery will remove that transverse process plus the nerve root near it and part of her rib. She will probably have numbness there because of the removal of the nerve root. They will insert at least 4 supporting hardware screws made out of carbon fiber. Carbon fiber is regularly used in Italy but still has not been approved by the FDA here in the US, so she is technically in a clinical trial for these and they are using them under an exemption. As I mentioned before, these will not cause the problems for further radiation treatments and imaging scans that traditional titanium screws would cause. They also hold up better to chemotherapy treatments than titanium, but we’re certainly hoping she doesn’t need any more of those.
Below is a diagram of the relevant areas of the spine. I circled in blue the areas that were removed in November and in red the area that will be removed next month.
Dr. Delaney, the radiation oncologist, will be treating Rachel with a radioactive iodine plaque placed directly on the dura (outside covering) of her spinal cord during surgery. There is a risk that the dura will tear during surgery, in which case they won’t be able to do this treatment because the radiation would make it so the tear wouldn’t heal properly. The doctors have mentioned that they think there might be some cancer cells on the dura itself, so we are certainly hoping that they are able to do this treatment. Dr. Delaney is the doctor who pioneered this sort of treatment. Mass General was therefore the first hospital to do this treatment (and may actually still be the only one doing it.)
Dr. Bojovic, the plastic surgeon, will be in the operating room to assist with closing the incision. Since she’s had a previous surgery in the area and has had radiation on that area, there’s a risk that there’s not enough good skin on her back to close the incision. It’s possible she will need a skin graft, but he doesn’t think so. The procedure he thinks she needs involves taking the lattisimus dorsi muscle on her back and detaching part of it and flipping it around to help cover the spine and hardware screws. This is a similar procedure to what they do in breast reconstruction surgery, though obviously her muscle only needs to move a little bit and not all the way around to her chest. Dr. Bojovic is the chief of plastic surgery at Shriners Children’s Hospital in Boston, in addition to working at Mass General.
The surgery will last most of the day and is the only surgery that her team has scheduled that day. Dr. Schwab estimated that they will be done around mid-afternoon, though Dr. Bojovic estimated early evening. If she’s under anesthesia for 8 or more hours, they will probably have her stay in the ICU for a while after surgery. Her length of stay in the hospital depends on how the surgery goes, how much the plastic surgeon needs to do, how quickly she recovers, etc. They said to plan on at least 3 nights in the hospital and up to a week or more. There’s a possibility she will need to go to a rehab facility afterward. Her post-op appointment is scheduled for September 21 and Dr. Schwab indicated it would be reasonable to stay in Boston until after that appointment, so we are probably going to do that. Rachel will have to avoid bending, lifting, and twisting (the BLTs, they said) after surgery, but they want her to do lots of walking.
We requested copies of her recent CT, bone, and MRI scans so that we could bring them to Boston with us. Dr. Schwab wants her to have another MRI at Mass General prior to surgery, as their MRI machine is much more detailed than Maine Med’s (shocker, right?) We received written final reports on the CT and bone scans with our scan copies. The CT scan report reads, “There are no suspicious nodules/masses to suggest pulmonary metastatic disease.” The CT report did mention that her heart suggested an “underlying element of anemia”, which we already knew from her blood tests. The report mentions “interstitial thickening” in her right lung that “might be related to radiation near this region.” We’re not sure what this means, so we will ask about it at her appointment with Dr. Weiss on Tuesday. The bone scan report states that there is “reduced but persistent uptake seen in the left T4 transverse process when compared with the last exam. No new or progressive findings”, which means that there are still cancer cells showing up, but less than before and the cancer has not spread to any other bones.
Rachel’s hemoglobin and platelets kept going down this week; she had to have blood tests on Monday, Wednesday, and Friday, to make sure she didn’t need transfusions. Yesterday’s results showed that they finally seem to be on the rise and she didn’t need any transfusions (borderline, but not quite low enough to be necessary.)
