As I mentioned last night, Rachel’s surgery was successful. The halo traction was helpful, but the surgeon still had a lot of work to do to get her spine back into alignment, causing the surgery to last about 7 hours instead of the anticipated 4. They were able to eventually get her spine back into a normal position, though, so that’s great news. There was a chance they wouldn’t be able to and would have to put in the supporting hardware with her upper spine still curved.
Prior to yesterday’s surgery the T3 vertebra (T=thoracic, middle section of the spine) was pushed forward, causing her spine to curve forward. They were able to get it pushed back into place, but it left a bit too much space going the other direction between T3 and T4 (T4 was where the tumor was.) To fill in the space, they used a cadaver bone from the bone bank. In September’s surgery, the surgeon tried to use as little hardware as possible to give Rachel the best range of motion and only put screws in T2 and T7, with rods in between. As we discovered, this wasn’t enough and the screws pulled out and caused the alignment problem. The surgeon had thought he would put the replacement hardware in the lower cervical spine (her neck), which would limit her movement more than the thoracic area. He ended up only putting screws in every vertebra from T1 through T7, with the exception of T4, which doesn’t have enough left of it to have supports. There are also rods in there as well. The new hardware is traditional titanium and not carbon fiber.
Here’s a spine diagram for reference:
Rachel didn’t have to go to the PICU after surgery this time; she was back in her regular room around 8:30 last night. She’s in quite a bit of pain, but with the halo gone she still seems better than before surgery. She also seems to be doing better than the surgery in September.
She was on bed rest and not able to elevate the head of her bed more than 30 degrees until they were able to get her brace refitted this morning. She has to wear that 24/7 for at least a couple days and then after that whenever she’s up and around for at least 6 weeks, though like before she can take it off to sleep and eat.
She has one small drain this time instead of the two larger ones she had in September. We’re told it should be removed fairly quickly and not left in for a couple weeks like last time. She’s already off IV fluids and IV pain meds, which took several days last time.
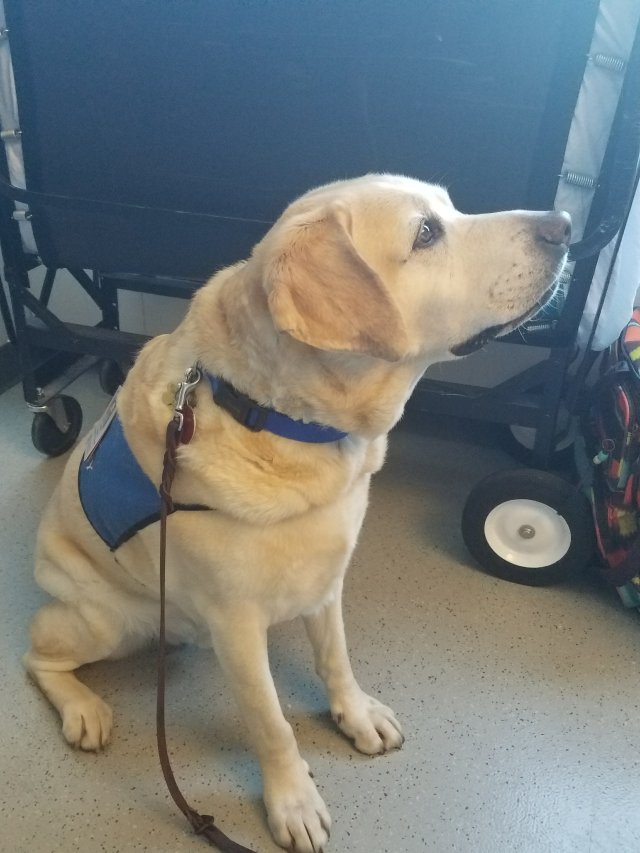
Rachel’s nurse getting all her “friends” back into bed, waiting for Rachel to come back and join them:


When Rachel was still in traction and having to lie in bed staring up toward the ceiling, the music therapist and child life specialist printed out some red panda pictures (her favorite animal) and hung them at the top of her curtain: